28th Aug 2020
What is Dissociation?

Our brain has various methods for coping with trauma and stress, one of these methods is dissociation.
When someone dissociates, their thoughts, feelings, behaviours, how they see their environment, memory, how present they are, and how they view the world disconnects. Their mind no longer works in harmony, and instead becomes separated. There are many theories of dissociation, but one is the idea that dissociation is a continuum, and that symptoms can range from mild to severe. In fact, for many of us, it may be a surprise to realise that we often mildly dissociate in our day-to-day life.
Dissociation for some may mean ‘zoning out’ or ‘daydreaming’ – it may present itself as missing your exit on the motorway or losing track of time during in a dull meeting. However, for someone who has experienced trauma, dissociation can show itself in a more pronounced way. It may impact their memory, sense of who they are, and how they perceive the world.
Severe dissociation may occur in many ways, such as forgetting past experiences, depersonalisation (feeling detached from yourself), or unusual experiences such as seeing/hearing things other people cannot. It may also cause vivid and realistic flashbacks to past trauma, whereby you feel like you’re ‘reliving’ a past experience. This can be a very frightening experience for the individual.
Dissociation is not a necessarily a bad thing though; it actually provides the individual with a psychological escape. It allows those who have experienced trauma to go about their normal daily living whilst coping with emotional distress. For some, many aspects of dissociating is a comforting, positive experience but it can also be a frightening reminder of upsetting experiences, causing your brain to jump into ‘panic mode’.
Caring for someone with dissociation, whether in a personal or professional capacity, may feel daunting. However, with understanding, you learn that they have simply found their own way to survive. Sometimes individuals get stuck an unhealthy habit to survive, which challenges their ability to recover from whatever they were trying to survive in the first place. Therefore, paying attention to dissociation is an important part of recovery.
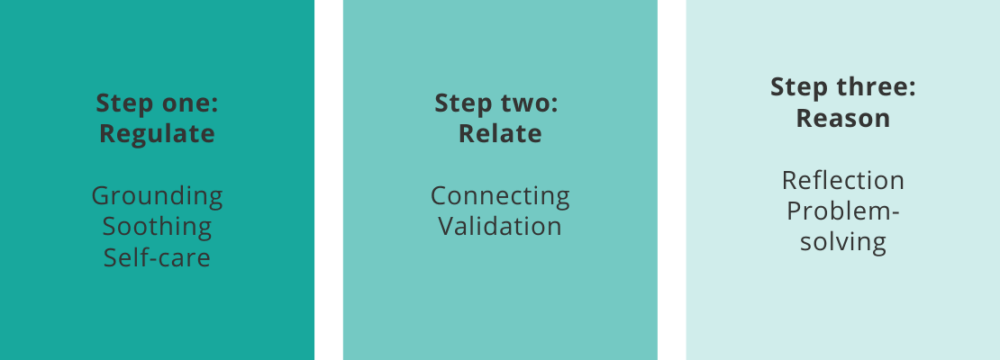
At Care in Mind, we use evidence-based methods for helping our young people in the most effective way. One of these methods is a three-step technique, based on regulating, relating, and reasoning. This can especially help during a flashback.
For regulation, the purpose is to help the individual to manage their response to the flashback. This may be done through encouraging grounding techniques. A comforting smell, relaxing song or hot drink may help assist someone in their grounding. It is also helpful to remind the individual that they are safe, and that the flashback will pass. Additionally, it is also important to promote self-care and soothing methods at this stage.
The second step, relating, is about connecting to the individual by being sensitive to their needs. We do this primarily through validation, which is a key element of our model of care. Validation is all about recognising someone’s feelings and allowing them to feel heard. However, it goes beyond words – it’s also about seeing and hearing the young person and connecting with them and their distress.
Finally, it is important to help the individual reflect on what just happened. It is at this point that, together, you can both reflect on what happened and what may help going forward. It can be useful to make a note of triggers and consider why your brain had the response that it did. At Care in Mind, it would be the young person’s assigned therapy session where they may do further reflecting on the incident, and thus find methods to avoid future episodes.
Dissociation is a normal and understandable coping response but if you find that it is causing you distress, please seek support. There are also ways in which you can care yourself. The mental health charity, Mind, has several helpful suggestions and information about coping with dissociation.
The content of this blog post is a summary of a recent webinar facilitated by Dr Lena Marden and Dr Christy Laganis, Clinical Psychologists at Care in Mind.

