1st Mar 2022
Introducing Edge Brook

The eating disorder epidemic is something never far from the media, with news stories often detailing how referrals and hospital admissions continue to rise.
According to an article published by the Guardian, eating disorder referrals have seen a stark rise during the pandemic of 2020/21, with lockdown causing eating disorders to thrive and available treatment being significantly impacted by pandemic-related issues. Additionally, the number of routine referrals rose from 915 in April to June 2016 to 1,850 in the first three months of 2020, this number then continued to rise to a record high from July to September, as it went up to 2,001. This data is based on routine referrals starting treatment in the community for children and young people. However, even prior to the pandemic, referrals have been rising, with a NHS Digital press release based on the Health Survey for England finding that 19% over women aged 16 and over screened positive for a possible eating disorder when question on their relationship with food in 2019. The same survey also found that almost one in eight men also screened positive for an eating disorder. This ongoing epidemic is clear when reviewing the eating disorder hospital admission statistics for 2018-19, which not only highlights the growing number of young people diagnosed with eating disorders, but also the amount that fall into the more complex category of ‘Other’, where they don’t fit into the bulimia or anorexia category.
Introducing Edge Brook
At Care in Mind we have spent the last few years working on developing a specialist service for young people with complex eating disorders. Over the years, we have seen ourselves the truth behind the headlines and statistics, and witnessed the increase in demand across eating disorder services and stretched capacity nationwide for Specialist Eating Disorder Unit (SEDU) inpatient beds. During this time period our own data also shows an increase in referrals for our core services for young people with a primary diagnosis of an eating disorder, or comorbidity with complex mental health needs.
In 2021 we opened Edge Brook, our first specialist residential service for young people with complex eating disorders. The service has been built on our core model of care, with additional specialised support for eating disorders.
Our commitment to least restrictive practice and the way in which we care for young people will reflect our core service offer. Therefore, there is an expectation that young people are of stable physical health and have managed at least 6 weeks without tube feeding by admission. Not only is this to ensure we can care for residents in the most therapeutic, least restrictive environment, but also to provide the best chance for a successful journey through our pathway to independence at a time when the young person is ready.
Developing Edge Brook was a lengthy process. We engaged in research in many forms, and held consultation sessions to gain insight from individuals, and their parents/carers, who have been treated by community and inpatient eating disorder services. These sessions were run by our Service User Coordinator who is also an expert by experience, and our Clinical Director. Individuals were given a chance to openly discuss their thoughts and feelings about the service following a brief explanation of our model of care for the service. Additionally, we worked closely with a dietician to gain valuable and specialist advice towards helping us to develop protocols.

Consultation Event Feedback
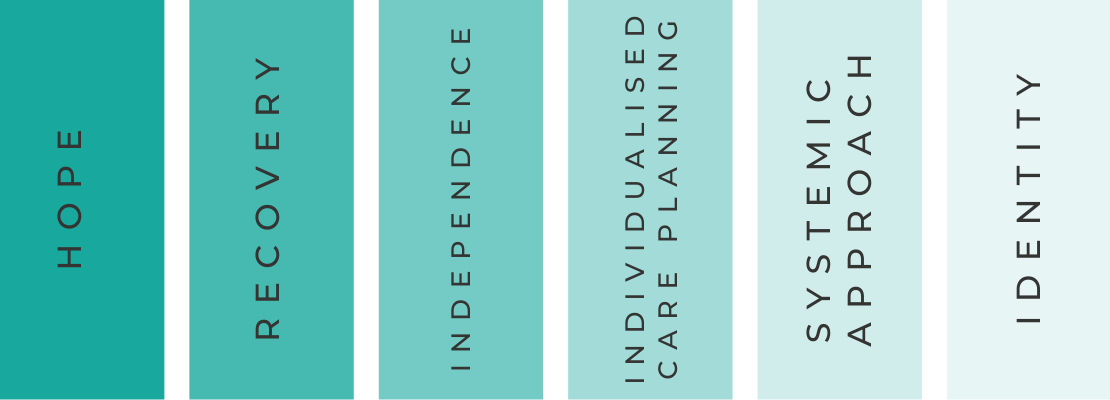
The research gathered during the consultation event was invaluable and gave us an important insight into what is truly required from an effective eating disorder service. Several key themes emerged from the feedback:
Hope: One of the strongest themes identified was the importance of hope, particularly when in inpatient settings where young people may feel stuck, and it can be difficult to be hopeful for the future and a life outside of hospital. Often young people in hospital with eating disorders can be subject to lengthy inpatient stays, or become ‘revolving door’ patients which may be down to a lack of appropriate pathways out of hospital. Giving young people the hope of a community-based residential treatment option could positively impact their motivation to move on from hospital.
Recovery: Another key theme was the importance of recovery from a ‘whole-person’ perspective. Participants felt that often there is an understandable focus on stabilisation of physical health but they felt it was important for services to consider what recovery means for each individual, and thinking about developing a sense of agency and achievement outside of their Eating Disorder identity. Ways we may do this include giving them more control over their lives, something we already do in our core residential homes, so that they are able to make decisions such as when they want to see their friends or what education they want to access. It’s important that young people are given this space for independence so that they can re-learn and build up their confidence in how to do everyday tasks that may have been done for them whilst in hospital.
Independence: Ensuring the building of independence skills will be a core focus, and it is important this is done in a way that meets people at their current level. Many of the young people we work with may feel de-skilled in many areas following lengthy inpatient stays and it is important that independence goals are developed around their needs and priorities. As with all elements of our service planning, the person-centred nature of this is key.
Individualised Care Planning: Individualised care planning is incredibly important to the way in which we work at Edge Brook. We believe eating disorders cannot be treated with one single approach, particularly when working with individuals with different diagnoses. Recovery goals for each individual are tailored, based on maintaining and developing their own physical health and independence-related goals. Goals are developed in collaboration with young people to support their understanding of exactly why we do what we do, and why this will benefit their journey to recovery. Additionally, we take the time to explain to young people why it is that everyone in the home has differing goals and care plans, but that everyone will receive the same high level of input and support.
Systemic Approach: Our participants highlighted the importance of joined up and consistent care, both within and across systems. At Edge Brook, building relationships and collaboration with local stakeholders is essential; particularly where a young person may require a short term re-admission to hospital to support stabilising their physical health. With collaboration, effective communication and clear joint working protocols, our hope is that admissions are short with a joined-up approach, supporting the young person to return to Edge Brook in a safe, structured and planned way.
Identity: The final key theme that emerged from the consultation event was Identity and in particular, who the young person is regardless of their eating disorder. Often young people who have had extensive inpatient admissions can feel robbed of key developmental stages in their adolescence which can lead to struggling with their identity outside of being a patient. Enabling young people to develop an identity is important whether that’s through giving our young people the ability to decorate their own rooms or supporting their interests in a new hobby.
The Home & Staffing Model
In many ways, our staffing model for Edge Brook reflects that of our core homes, however, as this is a specialist eating disorder home, we have additional specialist staff to support the complex and differing needs of the young people. We provide dietetic input through a specialised dietitian as well as in-house chefs to help young people create healthy, balanced meals (where appropriate). The home has increased physical health monitoring in comparison to our core service. This will be to ensure we are maintaining the physical aspect of the young people’s health as well as the psychological side of their recovery. Staff who work within the home have been carefully selected, to ensure that the right people are chosen for what is a challenging job. Like with our core service, staff are well supported through regular staff support sessions and reflective practice in addition to standard supervision, as we know that supported, happy staff are more effective in supporting the young people.
As with all of our homes, Edge Brook has a homely, caring feel and our young people are given a say in how to decorate both common areas and their own rooms. Furthermore, outside the home, there is a wealth of green space, including a duck pond and allotment. This will provide a mindful space for young people.

To make a referral or to find out more information about our services, please call the team on 0161 638 3285 or email referrals@careinmind.com

